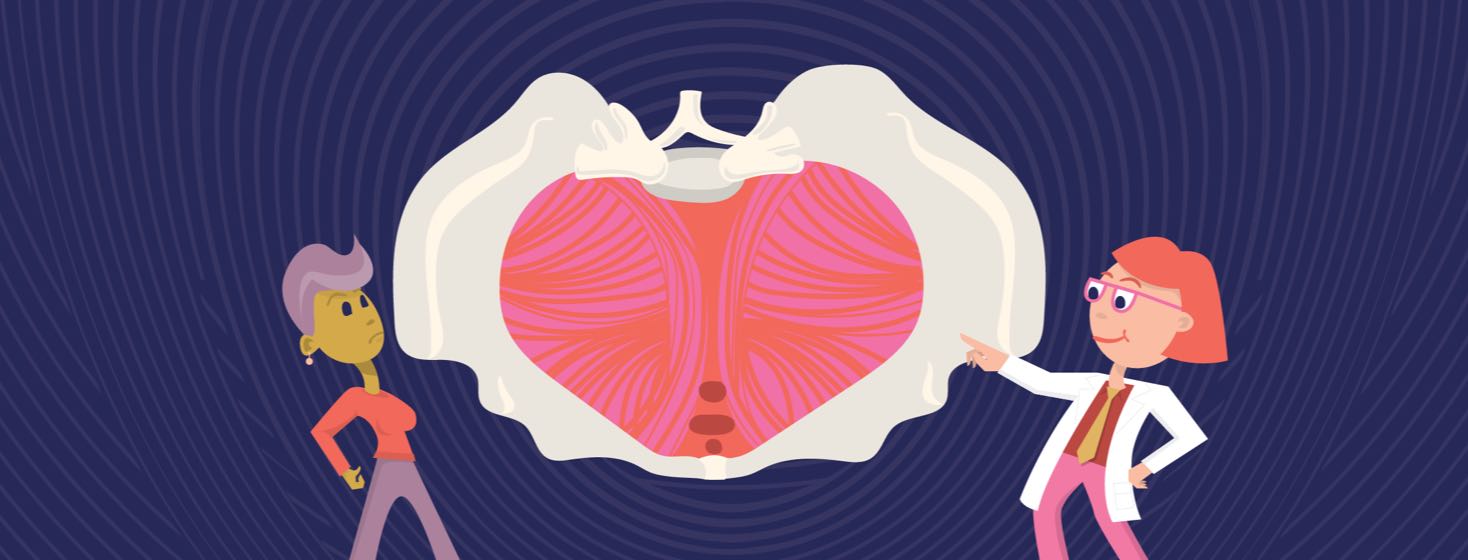
Pelvic Floor Prolapse: Should You be Worried?
If you have bladder cancer, your doctor might recommend a procedure called a radical cystectomy. During a radical cystectomy, doctors remove your bladder. They may also remove your surrounding organs since bladder cancer tends to spread. In women, these organs include:1
- Ovaries
- Fallopian tubes
- Uterus
- Cervix
- Part of the vagina
A radical cystectomy can weaken the pelvic floor muscles. It can also cause the small intestine and large intestine to protrude through the vaginal wall. This causes what is known as pelvic floor prolapse.1
What is pelvic floor prolapse?
Pelvic floor prolapse is a common condition affecting women. It happens when one of your pelvic organs moves from its original position and presses on your vagina. This can occur when the muscles in the pelvic floor have become too stretched or weak to support the pelvic organs.2
Pelvic organs include the:2
- Bladder
- Urethra
- Uterus
- Vagina
- Small bowel
- Rectum
What causes pelvic floor prolapse?
Anything that weakens pelvic muscles and tissues can cause pelvic floor prolapse. This can include:2
- Pregnancy and vaginal childbirth
- Giving birth to a large baby
- Obesity
- Increasing age and hormonal changes during menopause
- Family history of pelvic floor prolapse
- Repeatedly lifting heavy objects
- Chronic coughing due to lung disease or smoking
- Frequent constipation
- Previous surgery to fix a prolapsed organ
Women of all ages can experience pelvic floor prolapse. However, the condition mainly affects women over the age of 65 who have had 1 or more babies via vaginal childbirth.2
The link between bladder cancer and prolapse
There is limited research on the link between bladder cancer and pelvic floor prolapse in women. A 2021 study found that radical cystectomy for uroepithelial bladder cancer was not linked to an increased risk of pelvic organ prolapse in women. However, this study was small, and more research is needed to better understand any possible link.4
What are the symptoms?
Symptoms of pelvic floor prolapse vary depending on the severity of the prolapse. One of the most common symptoms is feeling pressure against your vaginal wall. It also may feel that your belly is unusually full. Other signs of pelvic floor prolapse include:2
- Lower back pain
- Vaginal spotting or bleeding
- Feeling constipated or losing control of your bowels
- Feeling like something is coming out of your vagina
- Pain or pressure in the pelvis or lower back
- Leaking urine when you cough, sneeze, or exercise
- Pain during sex
Symptoms of a prolapsed pelvic floor may interfere with your quality of life. The condition can cause physical discomfort along with social and mental stress.3
How is pelvic floor prolapse diagnosed?
To diagnose a prolapsed pelvic organ, your doctor will first do a pelvic exam. They may then use tests to look for issues with your pelvic organs, including:1,2
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Ultrasound
How is pelvic floor prolapse treated?
Treatment for pelvic floor prolapse varies and depends on factors like:2
- The severity of the prolapse
- The severity of your symptoms
- Your age and health
- Personal preferences
Your doctor might first suggest non-surgical treatment, like exercises to strengthen your pelvic floor muscles. They may also recommend losing weight if you are carrying extra pounds or adding more fiber to your diet if you suffer from chronic constipation.2
A pessary is another non-surgical treatment used for pelvic floor prolapse. It is a plastic or rubber removable device that is inserted into the vagina to support the pelvic organs.2
If your case is severe, your doctor may recommend surgery to repair the weakened pelvic floor tissues. In some cases of uterine prolapse, doctors may remove the uterus (hysterectomy).2

Join the conversation